Thursday, 30 November 2017
Paulskullate: WHAT IS TEMPOROMANDIBULAR JOINT DISORDER?
Paulskullate: WHAT IS TEMPOROMANDIBULAR JOINT DISORDER?: Temporomandibular joint disorder (TMJ disorder) is pain in the joint where your jaw meets your skull, just in front of your ears. TMJ disor...
WHAT IS TEMPOROMANDIBULAR JOINT DISORDER?
Temporomandibular joint disorder (TMJ disorder) is pain in the joint where your jaw meets your skull, just in front of your ears. TMJ disorder is more common in women than men.
WHAT IS THE CAUSE?
The cause of TMJ disorder is not known. Possible causes include:
Clenching your jaw or grinding your teeth. You may clench your jaws or grind your teeth when you are feeling stressed or when you are sleeping. If you do it mainly when you are sleeping, you may not even know you are doing it.
Dentures that do not fit properly
Frequent chewing of gum or ice
Physical or dental problems, such as teeth that don’t fit together properly or problems with the shape of your jaw
Swelling and irritation caused by arthritis or injury.
WHAT ARE THE SYMPTOMS?
The most common symptom is pain in your jaw joint, usually on one side only. The pain is usually dull but sometimes it may be sharp. In most cases the pain is worse when you move your jaw, especially when you are chewing. If you grind your teeth at night, the pain may be worse when you wake up in the morning.
Other symptoms may include:
Clicking, popping, or grating sounds when you move your jaw
Trouble completely opening your jaw or pain when you bite down
Headache
Ear pain or earache
The symptoms of TMJ disorder are similar to the symptoms of other conditions, such as ear problems. You should see your healthcare provider to find out what is causing your symptoms.
HOW IS IT DIAGNOSED?
Your healthcare provider will ask about your symptoms, activities, and medical history and examine you. You may have an X-ray.
HOW IS IT TREATED?
If there is a problem with the way your teeth fit together when you bite, your healthcare provider may refer you to a dentist. Your dentist may make a hard splint for you to wear during the day to keep your jaw from closing completely.
Your healthcare provider may give you a shot of steroid medicine to lessen any swelling and irritation caused by arthritis or an injury.
Other treatments may include:
Taking muscle relaxants for a few days
Practicing relaxation techniques
Learning ways to manage stress
Your healthcare provider may refer you to a physical therapist for treatment, such as massage and exercises that gently stretch the muscles and help with relaxation. If your pain is related to stress, counseling and medicine can help.
Surgery is rarely needed.
HOW CAN I TAKE CARE OF MYSELF?
To help relieve your symptoms:
Avoid overusing your jaw. You can rest your jaw by eating only soft food. Do not chew gum or ice.
Try not to clench your jaw or grind your teeth. Your healthcare provider may recommend a bite block (also called a night guard). A bite block is a plastic mouthpiece that stops your teeth from grinding together. It’s usually worn only at night.
Put a warm, moist washcloth on your jaw for 20 minutes, 4 to 8 times a day. Do not use a dry heating pad.
Massage the joint by pressing gently with your fingertips and moving them in a circular direction.
Ask your healthcare provider about taking a nonprescription pain medicine.
Follow the full course of treatment prescribed by your provider. Ask your provider:
How and when you will hear your test results
How long it will take to recover
What activities you should avoid and when you can return to your normal activities
How to take care of yourself at home
What symptoms or problems you should watch for and what to do if you have them
Make sure you know when you should come back for a checkup.
HOW CAN I HELP PREVENT TMJ DISORDER?
Because the cause of TMJ disorder is often not known, it can be hard to prevent. But the following may help:
Don’t chew a lot of gum or ice.
Try not to grind your teeth.
See your dentist for treatment if your teeth do not fit together well when you chew.
Wear proper protective head gear that fits well in all contact sports.
You can get more information from:
American Dental Association800-621-8099 http://www.mouthhealthy.org/en/
Developed by RelayHealth.
Published by RelayHealth.
Copyright ©2014 McKesson Corporation and/or one of its subsidiaries. All rights reserved.
Copyright google images
Copyright exercises http://melbournetmjcentre.com.au/tmj-exercises/
WHAT IS THE CAUSE?
The cause of TMJ disorder is not known. Possible causes include:
Clenching your jaw or grinding your teeth. You may clench your jaws or grind your teeth when you are feeling stressed or when you are sleeping. If you do it mainly when you are sleeping, you may not even know you are doing it.
Dentures that do not fit properly
Frequent chewing of gum or ice
Physical or dental problems, such as teeth that don’t fit together properly or problems with the shape of your jaw
Swelling and irritation caused by arthritis or injury.
WHAT ARE THE SYMPTOMS?
The most common symptom is pain in your jaw joint, usually on one side only. The pain is usually dull but sometimes it may be sharp. In most cases the pain is worse when you move your jaw, especially when you are chewing. If you grind your teeth at night, the pain may be worse when you wake up in the morning.
Other symptoms may include:
Clicking, popping, or grating sounds when you move your jaw
Trouble completely opening your jaw or pain when you bite down
Headache
Ear pain or earache
The symptoms of TMJ disorder are similar to the symptoms of other conditions, such as ear problems. You should see your healthcare provider to find out what is causing your symptoms.
HOW IS IT DIAGNOSED?
Your healthcare provider will ask about your symptoms, activities, and medical history and examine you. You may have an X-ray.
HOW IS IT TREATED?
If there is a problem with the way your teeth fit together when you bite, your healthcare provider may refer you to a dentist. Your dentist may make a hard splint for you to wear during the day to keep your jaw from closing completely.
Your healthcare provider may give you a shot of steroid medicine to lessen any swelling and irritation caused by arthritis or an injury.
Other treatments may include:
Taking muscle relaxants for a few days
Practicing relaxation techniques
Learning ways to manage stress
Your healthcare provider may refer you to a physical therapist for treatment, such as massage and exercises that gently stretch the muscles and help with relaxation. If your pain is related to stress, counseling and medicine can help.
Surgery is rarely needed.
HOW CAN I TAKE CARE OF MYSELF?
To help relieve your symptoms:
Avoid overusing your jaw. You can rest your jaw by eating only soft food. Do not chew gum or ice.
Try not to clench your jaw or grind your teeth. Your healthcare provider may recommend a bite block (also called a night guard). A bite block is a plastic mouthpiece that stops your teeth from grinding together. It’s usually worn only at night.
Put a warm, moist washcloth on your jaw for 20 minutes, 4 to 8 times a day. Do not use a dry heating pad.
Massage the joint by pressing gently with your fingertips and moving them in a circular direction.
Ask your healthcare provider about taking a nonprescription pain medicine.
Follow the full course of treatment prescribed by your provider. Ask your provider:
How and when you will hear your test results
How long it will take to recover
What activities you should avoid and when you can return to your normal activities
How to take care of yourself at home
What symptoms or problems you should watch for and what to do if you have them
Make sure you know when you should come back for a checkup.
HOW CAN I HELP PREVENT TMJ DISORDER?
Because the cause of TMJ disorder is often not known, it can be hard to prevent. But the following may help:
Don’t chew a lot of gum or ice.
Try not to grind your teeth.
See your dentist for treatment if your teeth do not fit together well when you chew.
Wear proper protective head gear that fits well in all contact sports.
You can get more information from:
American Dental Association800-621-8099 http://www.mouthhealthy.org/en/
Developed by RelayHealth.
Published by RelayHealth.
Copyright ©2014 McKesson Corporation and/or one of its subsidiaries. All rights reserved.
Copyright google images
Copyright exercises http://melbournetmjcentre.com.au/tmj-exercises/
Wednesday, 29 November 2017
OSTEOARTHRITIS PAIN RELIEF AND REPAIR WITH STEM CELL PROLOTHERAPY
Osteoarthritis is a chronic and debilitating joint disease. It occurs through a sequence of events that has, at its core, a loss of joint cartilage. This affects other joint structures, and eventually will lead to joint space narrowing and bony overgrowth, progressing until joint movement becomes noticeably restricted.
What occurs before the cartilage loss? Osteoarthritis almost always begins with ligament weakness or injury. Joints are composed of two bones covered with articular cartilage. Healthy ligaments hold the bones together and, along with the cartilage, enable the bones to glide evenly over one another. When the ligaments are weak, the bones will glide over one another in an uneven manner, causing one area of bone to bear additional weight on the articular cartilage.
Articular cartilage has no blood supply, and therefore, tends to heal slowly and imperfectly. Cartilage also lacks a neural network and does not elicit pain itself. The pain in osteoarthritis occurs from the pressure on the subchondral bone after the loss of cartilage tissue and from the stress on the tendons and ligaments of the joint.
Treatments for Osteoarthritis
There are many medications and procedures that temporarily relieve or mask the pain of arthritis. Non-steroidal anti-inflammatory drugs (NSAIDs), for instance, can accelerate the degeneration of the joints because they inhibit the normal tissue repair process.1 (See Figure 1.) Exercise, physical therapy, and lifestyle modification may provide symptom relief or surrounding muscle improvements, but they do nothing to regenerate the joint itself. There are, however, treatments available that stimulate the regenerative processes in the joint to facilitate the restoration of degenerated cartilage. One regenerative technique that has shown success is Stem Cell Prolotherapy. This is a natural injection treatment option that supplies the affected joint with chondrogenic (cartilage forming) stem cells and growth factors from a person’s own bone marrow and/or fat cells. Stem cells are in abundance in these tissues and have the ability to become various types of cells. Ongoing research and clinical evidence shows that injecting these cells into the degenerated joint supports chondrogenesis (the process by which cartilage is developed). (See Figure 2. )
Caring Medical Regenerative Medicine Clinics has performed several studies from its own patient population who have pain and/or osteoarthritis and opted for Prolotherapy and Stem Cell Prolotherapy instead of joint surgery. One study of seven patients with hip, knee or ankle osteoarthritis and another cohort comprised of 24 patients who had been clinically diagnosed with radiographic osteoarthritis. 2,3 The treatments comprised of dextrose Prolotherapy in and around the involved joint as well as stem cell/bone marrow aspirate injections in and around the arthritic joints.
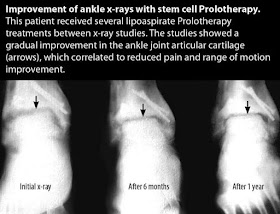
Dextrose Prolotherapy itself is a technique that is used to aid the body in healing by prompting it to create new collagen. Numerous studies have shown the effectiveness of dextrose Prolotherapy in treating osteoarthritis, as well as ligament and tendon injuries.4-7 Prolotherapy offers benefits in terms of pain relief, regenerative properties, and cartilage repair for people affected by musculoskeletal disorders. Dextrose Prolotherapy involves the injection of a hypersmolar dextrose solution into an injury site to elicit localized inflammation, which is the first step in healing the damaged area. The dextrose solution acts as a proliferant via the induction of local healing cascades. With the addition of the cellular solutions, the goal is to improve treatment outcomes in patients with advanced osteoarthritic conditions, including those evidenced by X-ray. (See X-rays.)
Prolotherapy provides a safe and effective regenerative treatment option for osteoarthritis, one that has demonstrated the potential to slow down the progression of osteoarthritis and one that promotes the regeneration of articular cartilage… essentially a new paradigm in the treatment of osteoarthritis.
What occurs before the cartilage loss? Osteoarthritis almost always begins with ligament weakness or injury. Joints are composed of two bones covered with articular cartilage. Healthy ligaments hold the bones together and, along with the cartilage, enable the bones to glide evenly over one another. When the ligaments are weak, the bones will glide over one another in an uneven manner, causing one area of bone to bear additional weight on the articular cartilage.
Articular cartilage has no blood supply, and therefore, tends to heal slowly and imperfectly. Cartilage also lacks a neural network and does not elicit pain itself. The pain in osteoarthritis occurs from the pressure on the subchondral bone after the loss of cartilage tissue and from the stress on the tendons and ligaments of the joint.
Treatments for Osteoarthritis
There are many medications and procedures that temporarily relieve or mask the pain of arthritis. Non-steroidal anti-inflammatory drugs (NSAIDs), for instance, can accelerate the degeneration of the joints because they inhibit the normal tissue repair process.1 (See Figure 1.) Exercise, physical therapy, and lifestyle modification may provide symptom relief or surrounding muscle improvements, but they do nothing to regenerate the joint itself. There are, however, treatments available that stimulate the regenerative processes in the joint to facilitate the restoration of degenerated cartilage. One regenerative technique that has shown success is Stem Cell Prolotherapy. This is a natural injection treatment option that supplies the affected joint with chondrogenic (cartilage forming) stem cells and growth factors from a person’s own bone marrow and/or fat cells. Stem cells are in abundance in these tissues and have the ability to become various types of cells. Ongoing research and clinical evidence shows that injecting these cells into the degenerated joint supports chondrogenesis (the process by which cartilage is developed). (See Figure 2. )
Caring Medical Regenerative Medicine Clinics has performed several studies from its own patient population who have pain and/or osteoarthritis and opted for Prolotherapy and Stem Cell Prolotherapy instead of joint surgery. One study of seven patients with hip, knee or ankle osteoarthritis and another cohort comprised of 24 patients who had been clinically diagnosed with radiographic osteoarthritis. 2,3 The treatments comprised of dextrose Prolotherapy in and around the involved joint as well as stem cell/bone marrow aspirate injections in and around the arthritic joints.
Dextrose Prolotherapy itself is a technique that is used to aid the body in healing by prompting it to create new collagen. Numerous studies have shown the effectiveness of dextrose Prolotherapy in treating osteoarthritis, as well as ligament and tendon injuries.4-7 Prolotherapy offers benefits in terms of pain relief, regenerative properties, and cartilage repair for people affected by musculoskeletal disorders. Dextrose Prolotherapy involves the injection of a hypersmolar dextrose solution into an injury site to elicit localized inflammation, which is the first step in healing the damaged area. The dextrose solution acts as a proliferant via the induction of local healing cascades. With the addition of the cellular solutions, the goal is to improve treatment outcomes in patients with advanced osteoarthritic conditions, including those evidenced by X-ray. (See X-rays.)
Prolotherapy provides a safe and effective regenerative treatment option for osteoarthritis, one that has demonstrated the potential to slow down the progression of osteoarthritis and one that promotes the regeneration of articular cartilage… essentially a new paradigm in the treatment of osteoarthritis.
TWELVE (12) THINGS TO REMEMBER IN LIFE
- THE PAST CANNOT BE CHANGED.
- OPINIONS DON'T DEFINE YOUR REALITY.
- EVERYONE'S JOURNEY IS DIFFERENT.
- THINGS ALWAYS GET BETTER WITH TIME.
- JUDGMENTS ARE A CONFESSION OF CHARACTER.
- OVERTHINKING WILL LEAD TO SADNESS.
- HAPPINESS IS FOUND WITHIN.
- POSITIVE THOUGHTS CREATE POSITIVE THINGS.
- SMILES ARE CONTAGIOUS.
- KINDNESS IS FREE.
- YOU ONLY FAIL IF YOU QUIT.
- WHAT GOES AROUND, COMES AROUND.
Saturday, 25 November 2017
FULL TEXT OF PROSTATE HEALTH AWARENESS LECTURE.
MEN - MY CHILDHOOD; MY MANHOOD; MY PROSTATE.. MUST READ!!
Ladies and Gentlemen
I am here to speak with you on Prostate. The topic is misleading. Is prostate strictly for men? Yes, ONLY men have prostate and ONLY men over 40years but the healthcare enlightenment is for everyone. There is no woman who does not know a man 40 years and above – father, uncle, brother, son, friend, neighbor, colleague …
Essentially what I will be doing today is health promotion. Responsible health promotion must provide three things:
1. Information
2. Reassurance
3. A plan of action.
Let me start with a background on prostate health.
Everyone has a pair of kidneys. The job of the kidney is to remove waste. It is the LAWMA (waste management company) of your body. Everyday your blood passes through the kidney several times to be filtered. As the blood is filtered, urine is formed and stored in a temporary storage tank called the urinary bladder.
If there were to be no urinary bladder, as a man walks on the road, urine will be dropping.
Now think of the plumbing work in your house. Think of the urinary bladder as the overhead storage tank. From the storage tank, a good plumber will run pipes to other parts of the house, including the kitchen. God in His wisdom ran pipes from our urinary bladder to the tip of the penis. The pipe is called the urethra. Just below the bladder and surrounding the urethra is a little organ called the prostate gland.
The prostate gland is the size of a walnut and weighs about 20grams. Its job is to make the seminal fluid which is stored in the seminal vesicle. During sexual intercourse, seminal fluid comes down the urethra and mixes with the sperms produced in the testicles to form the semen. So semen technically is not sperm. It is sperm + seminal fluid. The seminal fluid lubricates the sperm.
After age 40, for reasons that may be hormonal, the prostate gland begins to enlarge. From 20 grams it may grow to almost 100 grams. As it enlarges, it squeezes the urethra and the man begins to notice changes in the way he urinate.
If you have a son under 10, if he has a little mischief like we all did at that age, when he comes out to urinate, he can target the ceiling and the jet will hit target. Call his father to do same, wahala dey. His urine stream is weak, cannot travel a long distance and sometimes may come straight down on his legs. So he may need to stand in awkward position to urinate.
Not many men will be worried their urine stream cannot hit the ceiling. Toilets are on the floor and not on the ceiling. But other symptoms begin to show.
TERMINAL DRIPPLING:
The man begins to notice that after urinating and repacking, urine still drops on his pants. This is the reason why after an older man urinates, he has to ring bell. A younger man simply delivers to the last drop and walks away. Just see an older man coming from the bathroom. Sometimes he may clutch the newspaper closely to hide the urine stains, particularly on plain colored trousers.
HESISTANCY
At this point you wait longer for the urine flow to start. There are 2 valves that must open for you to urinate – the internal and external sphincters. Both open but because of obstructions in the urethra, you wait long for the flow to start.
INCOMPLETE EMPTYING
You have this feeling immediately after urinating that there is still something left.
As all these things happen, the bladder begins to work harder to compensate for the obstruction in the urethra. The frequency of urination goes up. Urgency sets in. sometimes you have to practically run into the toilet. Nocturia also becomes common. You wake up more than 2 times at night to urinate. Your wife begins to complain.
Men being men may not talk to anyone even at this point. Then the more serious complications start.
Stored urine gets infected and there may be burning sensation when urinating.
Stored urine forms crystals. Crystals come together to form stone either in the bladder or in the kidney. Stones may block the urethra.
Chronic urinary retention sets in. The bladder stores more and more urine. The size of the bladder is 40 - 60 cl. A bottle of coke is 50cl. As the bladder stores more urine it can enlarge up to 300cl. An overfilled bladder may leak and this leads to wetting / urinary incontinence. Also the volume may put pressure on the kidney and may lead to kidney damage.
What may likely bring the man to hospital is acute urinary retention. He wakes up one day and he is not able to pass urine.
Everything I have described above is associated with prostate enlargement, technically called benign prostate hyperplasia.
There are other diseases of the prostate like:
1. Prostatitis – inflammation of the prostate
2. Prostate cancer – cancer of the prostate.
This discussion is on prostate enlargement.
I have bad news and good news.
The bad news is that everyman will have prostate enlargement if he lives long enough.
The good news is that there are life style changes that can help the man after 40 to maintain optimum prostate health.
Nutrition
Look at what you eat. 33% of all cancers, according to the US National Cancer Institute is related to what we eat.
Red meat everyday triples your chances of prostate disease. Milk everyday doubles your risk. Not taking fruits / vegetables daily quadruples your risk.
Tomatoes are very good for men. If that is the only thing your wife can present in the evening, eat it with joy. It has loads of lycopene. Lycopene is the most potent natural antioxidant.
Foods that are rich in zinc are also good for men. We recommend pumpkin seeds (ugbogulu).
Zinc is about the most essential element for male sexuality and fertility.
Men need more zinc than women. Every time a man ejaculates he loses 15mg of zinc. Zinc is also important for alcohol metabolism. Your liver needs zinc to metabolize alcohol.
ALCOHOL CONSUMPTION
As men begin to have urinary symptoms associated with prostate enlargement, it is important they look at alcohol consumption. More fluid in means more fluid out.
Drink less. Drink slowly.
EXERCISE
Exercise helps build the muscle tone. Every man should exercise. Men over 40 should avoid high impact exercise like jogging. It puts pressure on the knees. Cycling is bad news for the prostate. We recommend brisk walking.
SITTING
When we sit, two-third of our weight rests on the pelvic bones. Men who sit longer are more prone to prostate symptoms. Do not sit for long hours. Walk around as often as you can. Sit on comfortable chairs. We recommend a divided saddle chair if you must sit long hours.
DRESSING
Men should avoid tight underwear. It impacts circulation around the groin and heats it up a bit. While the physiological temperature is 37 degrees, the groin has an optimal temperature of about 33 degrees. Pant is a no - no for men. Wear boxers. Wear breathable clothing.
SMOKING
Avoid smoking. It affects blood vessels and impact circulation around the groin.
SEX
Regular sex is good for the prostate.
Celibates are more prone to prostate illness. While celibacy is a moral decision, it is not a biological adaptation. Your prostate gland is designed to empty its contents regularly.
Thought: When someone shares something of value with you and you benefit from it, you have a moral obligation to share it with others.
#copied.